By Jon Roberts MD, Driscoll Children’s Hospital
Cystic fibrosis (CF) is a chronic, genetic disease that affects about 30,000 people in the United States, and 70,000 people worldwide. The defective gene found in CF patients causes the body to make thick mucus that can clog the lungs and lead to infection. It may also block the pancreas and keep natural enzymes from helping the body digest and absorb food.

A child with CF may experience a number of signs and symptoms, including the following:
- Wheezing or shortness of breath
- Frequent cough and increased lung mucus
- Multiple episodes of bronchitis and pneumonia
- Nasal polyps and frequent sinus infections
- Slow weight gain or weight loss, even with a healthy appetite
- Abnormal or frequent bowel movements
- Liver and gallbladder disease
- Enlargement of the fingertips and toes (clubbing)
- Rapid dehydration and heat stroke
- Fertility issues
The disease previously carried a life expectancy of less than 5 years of age, mainly due to malnutrition and failure to grow. With the advent of pancreatic enzyme replacement therapy in the early 1950s, patients were able to maintain good nutrition and growth, and the life expectancy jumped to about 10 – 15 years of age. With CF children surviving longer, it became apparent that the main issue would become chronic, worsening lung disease. Now able to live beyond the first few years, these children were succumbing to overwhelming airway and lung infections. Thus, the care of CF was handed over to pulmonary specialists.
“Over the past 60 years or so, doctors and scientists have revolutionized the management of children with cystic fibrosis.”
Over the past 60 years or so, doctors and scientists have revolutionized the management of children with cystic fibrosis. Airway clearance techniques (using specialized vests and other devices) have allowed patients to loosen the thick mucus in the airways and improve lung function. Inhaled medications, such as hypertonic saline and dornase alpha) have functioned to thin the mucous and help clear it from the lungs. Inhaled antibiotics have made it possible to more-efficiently kill disease-causing bacteria, such as Pseudomonas aeruginosa and Staphylococcus aureus.
These measures (giving digestive enzymes because the body cannot make its own, loosening and clearing thick mucus in sinuses and lungs) have pushed the life-expectancy of CF from less than 5 years of age in the 1950s, to just over 40 years of age today. In fact, 2015 marked the first year there were more adults living with cystic fibrosis than children – and the future is looking optimistic! In the last decade, new medications have been created to directly target the DNA and proteins that cause the disease in the first place. In 2012 the drug ivacaftor was approved for use in the United States, allowing the defective protein that causes the disease to work properly in about 5% of CF patients. In 2015, a second medication (a combination of the same ivacaftor and another called lumacaftor) was approved to treat the most common genetic cause of CF known as delta F-508 mutation. It is the hope of CF specialists around the world that a cure for the disease is on the horizon.
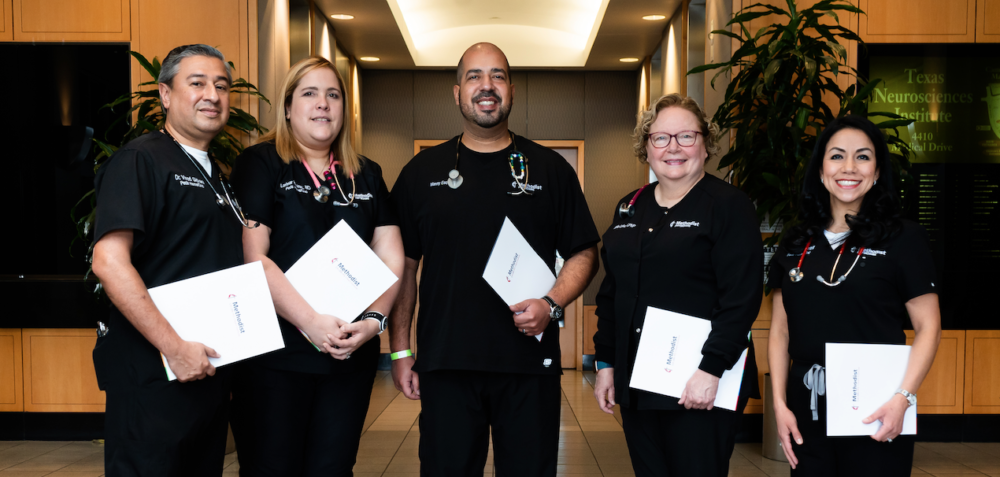
In 2015 the Driscoll Children’s Hospital Cystic Fibrosis Center became one of only 110 centers nationwide accredited as a Cystic Fibrosis Foundation Affiliate program. In doing so, it became the first cystic fibrosis center to serve the population of South Texas. Children with CF are urged to visit an accredited care center four times a year for visits which include evaluations with a physician, respiratory therapist, nutritionist and social worker. Driscoll’s earned accreditation makes it possible for patients living in South Texas to make those visits. The Driscoll Center houses an experienced team of physicians, respiratory therapists, nurses, dieticians, social workers, physical therapists and pharmacists ready to give patients the highest quality care available.



Recent Comments